- The most frequent indication for cholescintigraphy is to confirm or exclude the diagnosis of acute cholecystitis.
- Patients present with colicky right upper quadrant abdominal pain, nausea, and vomiting.
- Physical examination often detects right upper quadrant tenderness. Laboratory studies show leukocytosis.
- Series of sequential histopathological inflammatory changes occurs—first, venous and lymphatic obstruction, followed by edema of the gallbladder mucosa, then white blood cell infiltration, and, ultimately, hemorrhage, ulceration, necrosis, and if left untreated, gangrene, abscess, and perforation.
USG:
- Most patients with acute cholecystitis have gallstones noted on sonography; however, the presence of stones is not specific for acute cholecystitis.
- Asymptomatic gallstones are common and may be unrelated to the cause of the abdominal pain.
- Thickening of the gallbladder wall and peri-cholecystic fluid occur with various acute and chronic diseases.
- A more specific indicator of acute inflammation is intramural lucency. The sonographic Murphy sign (localized tenderness in the region of the gallbladder) is reported to have high accuracy in experienced hands; however, this finding is operator dependent and not always reliable. The combination of gallstones, intramural lucency, and the sonographic Murphy sign makes the diagnosis of acute cholecystitis likely.
- Ultrasonography may reveal other factors causing the patient’s symptoms (e.g., common duct dilation due to biliary obstruction, pancreatic or liver tumors, renal stones, pulmonary consolidation).
Cholescintigraphy
- A major advantage of HIDA scintigraphy is that it demonstrates the pathophysiology of acute cholecystitis (i.e., nonfilling of the gallbladder secondary to cystic duct obstruction).
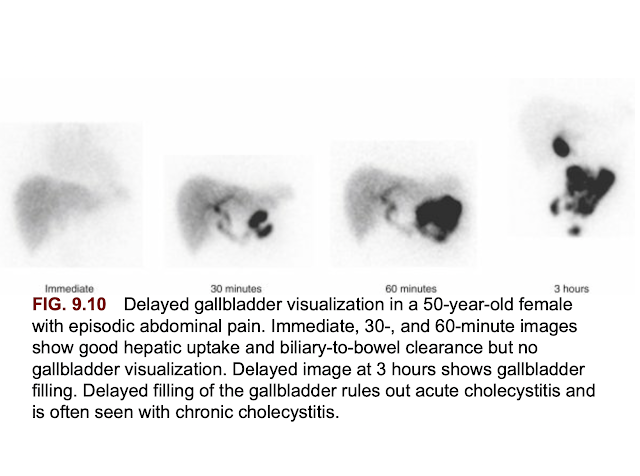
- No filling by 60 minutes after Tc-99m HIDA injection is abnormal; however, it is not, by itself, diagnostic of acute cholecystitis.
- However, no filling on further delayed imaging at 3 to 4 hours or 30 minutes after morphine infusion is diagnostic of acute cholecystitis.
- Delayed filling of the gallbladder (i.e., after 60 minutes) rules out acute cholecystitis. Common reasons for delayed gallbladder filling are chronic cholecystitis and hepatic dysfunction
- Cholescintigraphy has high accuracy for the diagnosis of acute cholecystitis. The sensitivity (nonfilling of the gallbladder in those with the disease) is 95% to 98%, and the specificity (filling of the gallbladder in patients who do not have the disease) is > 90%.
- Ensuring that patients have fasted for 3 to 4 hours before the study is critical. Those fasting > 24 hours or receiving hyperalimentation likely have a gallbladder full of viscous bile and should be administered sincalide before the study to empty the gallbladder.
False Positive
- In these cases, false positives may still occur because of a poorly contracting gallbladder in response to CCK due to chronic cholecystitis. Patients with poor hepatic function have delayed uptake and clearance of the radiotracer and often delayed gallbladder filling. In these patients, delayed imaging for up to 24 hours may be necessary to confirm or exclude gallbladder filling; false positives may still occasionally occur.
- Patients with chronic cholecystitis may have false-positive findings for acute cholecystitis (nonfilling of the gallbladder) caused by a fibrotic obstruction of the cystic duct or a functional obstruction caused by a gallbladder filled with viscous bile. Even if a patient has received sincalide before the study, a diseased gallbladder, whether acute or chronic, may not contract.
- Very ill hospitalized patients with a concurrent serious illness may also have false-positive scintigraphic results for acute cholecystitis. The reason for this is uncertain.
False Negative:
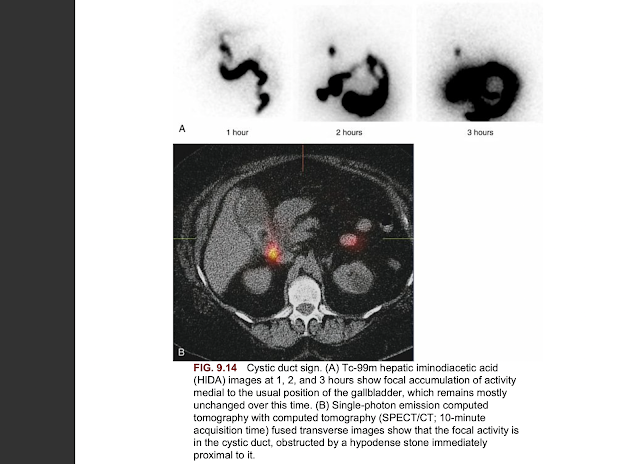
- False-negative results (gallbladder filling in a patient with acute cholecystitis) are rare. One important cause to be avoided is misinterpretation of the cystic duct sign, specifically cystic duct dilation proximal to its obstruction, which might be misinterpreted as a gallbladder. The focal activity is typically smaller than a gallbladder and in a more medial position
- If the gallbladder does not fill by 1 hour, either delayed imaging for up to 4 hours or morphine administration is indicated to confirm or exclude gallbladder filling.
Morphine Administration:
- The accuracy of morphine is similar to the delayed imaging method and is preferred whenever possible because it confirms or excludes the diagnosis by 30 minutes after administration.
- Morphine produces a functional partial common duct obstruction that cannot be differentiated by scintigraphy from a pathological partial common duct obstruction caused by stone or structure.
- Thus, morphine should not be administered if scintigraphic findings show delayed clearance from the common duct and delayed transit into the small bowel.
- Delayed imaging is indicated for these patients.
- With cystic duct patency, the gallbladder begins to fill within 5 to 10 minutes after morphine infusion and is complete by 20 to 30 minutes.
- If no gallbladder filling is seen by the end of the 30-minute infusion, acute cholecystitis is confirmed.
Ancillary Findings:
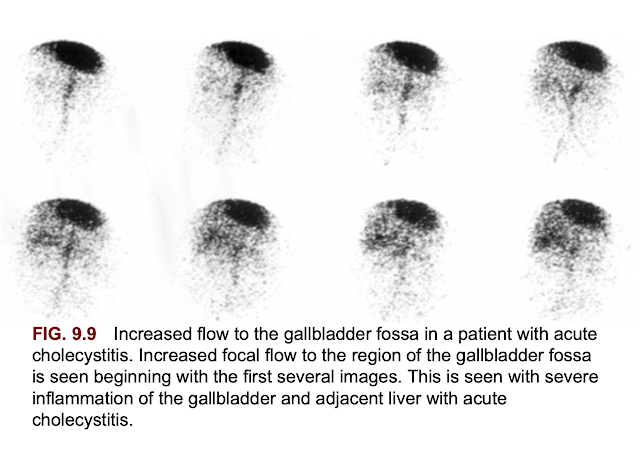
- Increased blood flow to the gallbladder fossa secondary to severe inflammation is seen in some patients.
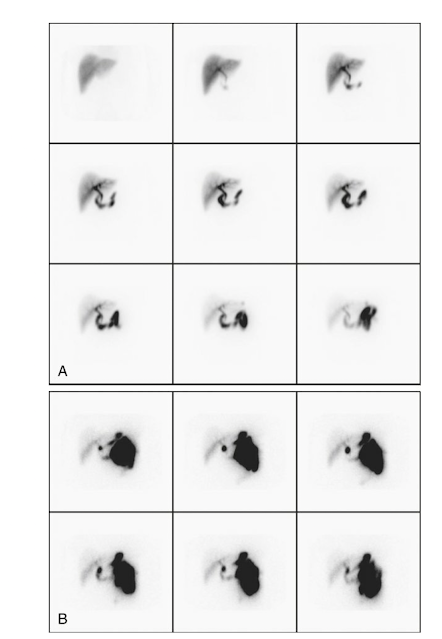
- Increased hepatic uptake of HIDA tracer adjacent to the gallbladder fossa in patients with acute cholecystitis is called the rim sign and is seen in approximately 25% of patients with acute cholecystitis. The rim sign is more common than increased flow to the gallbladder fossa. Sometimes they occur together. The rim sign can usually be seen throughout the duration of the study but is best seen as the radiotracer clears from the uninvolved liver.
- It is caused by inflammation of the liver adjacent to the gallbladder fossa.
- With severe acute cholecystitis, inflammation may spread to the adjacent normal liver, which can result in increased blood flow to that region, increased radiotracer delivery, and thus increased Tc-99m HIDA hepatic extraction.
- The importance of the rim sign is twofold.
- First, it is a very specific scintigraphic finding of acute cholecystitis. It increases interpretive confidence that nonfilling of the gallbladder is caused by acute cholecystitis (true positive) in a patient at increased risk for a false- positive study, for example, a sick hospitalized patient with concurrent serious illness.
- Second, the rim sign identifies patients with acute cholecystitis who have more severe disease and are at increased risk for complications (e.g., gangrene and perforation). Even without these complications, patients with the rim sign tend to be sicker and at a later stage of the pathophysiological spectrum of disease, with hemorrhage and necrosis rather than edema and leukocyte infiltration.