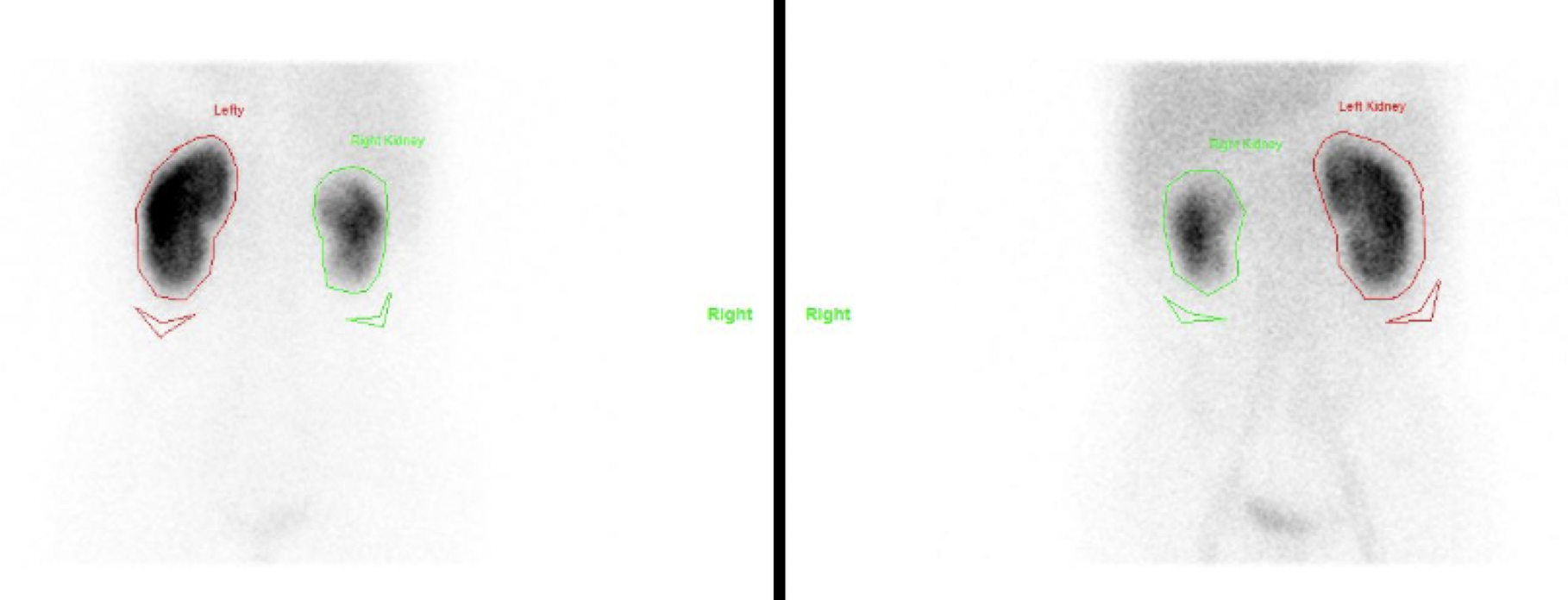
- Renal cortical scintigraphy image functional renal tissue and provide useful morphologic information
- 99mTc-DMSA and 99mTc-GH (glucoheptonate)
- Retained in the proximal tubules for a prolonged time after injection
- DMSA is commonly used due to higher retention (30% vs 5-10% of GH)
Indications:
- Acute pyelonephritis
- Cortical scarring
- Relative functioning renal mass
- Solitary or ectopic renal tissue (pelvic kidney)
- Horseshoe kidney
- To differentiate prominent column of Bertin from true mass
Tc99m DMSA
- Dimercaptosuccinic acid
- 40-50% of injected dose localizes in the cortex in PCT
- Imaging is done after 2-3 hours to allow time for slow background clearance
- Diseases affecting proximal tubules like renal tubular acidosis and Fanconi’s syndrome and nephrotoxic drugs like Cisplatin and Gentamicin inhibit DMSA uptake
- Dose – Children: 50 µCi/kg (minimum 0.6 mCi), Adult: 5 mCi
Procedure:
- Inject DMSA intravenously and acquire images after 2 hours
- Void before starting
- Acquire parallel hole collimater images in supine position for 500k counts or use fixed time of 5-10 mins/view in posterior and posterior oblique (30˚ - 35˚) views on 128 × 128 or 256 × 256 matrix
- Pinhole images acquire for 100k counts. Pinhole collimator provides magnification and improved resolution, allows detection of smaller cortical defects
- Horseshoe and pelvic kidneys are imaged anteriorly
- Quantify function as geometric mean
- Advise to maintain hydration and frequent bladder emptying after imaging to minimise radiation dose to kidneys and bladder
Interpretation:
- Normally homogenous distribution throughout cortex
- Upper poles may appear less intense due to splenic impression, fetal lobulation, attenuation from liver and spleen
- Areas of cortical tubular dysfunction from infection or scar present as cortical defects
- Infection may present as single or multifocal ill-defined defect – reduced or absent localization of tracer with indistinct margins that do not deform renal contour
- Scars have localized, sharp margins and may occur in a small kidney. Scarring can manifest as cortical thinning, flattening or an ovoid or wedge-shaped defect
- In a/c pyelonephritis, serial scans may be useful to assess extend of recovery (wait for 6 months after a/c infection)
- Defect persisting after 6 months should be considered chronic scar
- Tracer uptake is seen in column of Bertin but not in a mass
Source of error
- Flattening of superolateral aspect of left kidney may be attributed to splenic impression.
- Exaggerated contrast between intervening parenchyma and renal poles suggest erroneously bipolar hypoactivity.
- Air introduced into the reaction vial can degrade the DMSA complex resulting in decreased renal uptake and increased hepatic and background activity.